Previous Issue (Volume - 7 | Issue - 1)
Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trial
Published on: 3rd February, 2023
Objectives: To examine the effect of dietary supplements on diabetic risk progression, blood glucose level, and lipid profiles.Methods: A randomized, double-blind, placebo-controlled study was conducted at Rajavithi hospital, Thailand. Participants with prediabetes were randomly allocated to three arms of dietary supplements: placebo (PL) or curcumin plus fish oil and vitamin D (CFD), or curcumin plus fish oil (CF) for 24 weeks. Primary outcomes were the progression of glycemic status and the progression to overt diabetes at 24-week and 36-week follow-ups. Secondary outcomes were changes in glycemic profiles (fasting plasma glucose, 75 g OGTT 2-h plasma glucose or HbA1C), body weight, BMI and lipid profiles.Results: A total of forty-seven participants (PL, n = 16; CFD, n = 15; CF, n = 16) were included in the study. At the 24-week follow-up, the participants with worsening glycemic status in the intervention groups were lower, CFD, CF and Placebo, 14.29%, 13.33% and 31.25%, respectively. However, the primary outcome, progression of glycemic status, was statistically different, with p - value = 0.046 (p < 0.05) when excluding previous diabetes in the study. As well as the incidence of type 2 diabetes at 24-week follow-up was not statistically different between the three groups, 14.29%, 13.33%, and 12.5%, p - value = 0.699 (p < 0.05) in CFD, CF, PL group, respectively. The secondary outcomes also failed to demonstrate the effect of dietary supplements on blood glucose, lipid profiles, weight, BMI and blood chemistry.Conclusion: The combined dietary supplements which contained curcumin-fish oil-vitamin D,could lower the glycemic status progression in prediabetes at six months follow-up and were well-tolerated among the participants.
Myxedema Coma and Acute Respiratory Failure in a Young Child: A Case Report
Published on: 26th July, 2023
Background: Myxedema is an extreme manifestation seen in patients with untreated hypothyroidism. It is a lethal endocrine emergency, which arises when a precipitating cause overwhelms the compensatory mechanisms of the hypothyroid state.Objectives: This case report aims to present a case of myxedema coma secondary to cretinism. It also aims to discuss how hypothyroidism leads to hypoventilation and eventually respiratory failure, as well as to discuss the epidemiology, pathophysiology, clinical manifestation, diagnosis, and management of a child with myxedema coma.Case presentation: This is a case of a 7-year-old female, diagnosed with congenital hypothyroidism at 5 months of age, but eventually was lost to follow-up. She came back after 7 years presenting with difficulty of breathing. She was seen hypothermic, obtunded, and in severe respiratory distress. She was severely stunted and underweight with coarse facial features. Initial laboratory work-up showed elevated Thyroid Stimulating Hormone (TSH) as well as decreased tri-iodothyronine (FT3) and thyroxine (FT4). She was immediately started on levothyroxine, with noted resolution of the edema and improvement in sensorium. There was also noted improvement in the patient’s ventilation and was sent home on Continuous Positive Airway Pressure (CPAP) while asleep.Conclusion: This case highlights the importance of having a high index of suspicion of its clinical manifestations, which could lead to earlier intervention thereby preventing further complications. A multidimensional approach is essential in managing this case, as various organ systems are involved in this condition.
Evaluation of Thyroid and Lipid Profile of Hiv Patients Seen in a Faith-Based Health Facility in Anambra State, Nigeria
Published on: 1st August, 2023
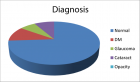
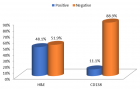
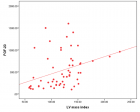
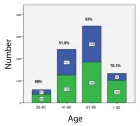
Background: Human Immunodeficiency Virus (HIV) and thyroid function have been described. Prevalence pattern and atherogenic status significantly differ from HIV-negative control in several studies. Unfortunately, few studies have determined the prevalence of thyroid function and lipids among Nigerians living with HIV. Objective: This study is to evaluate thyroid hormones and lipid profiles in HIV-positive subjects attending a faith-based health facility in Anambra State Nigeria.Materials and methods: The serum concentration of Thyroid Stimulating Hormone (TSH), free Triiodothyronine (fT3), triiodothyronine (T3), free Thyroxine (fT4), Thyroxine (T4), Total Cholesterol [TC], Triglyceride [TG], High-Density Lipoprotein [HDL], Low-Density Lipoprotein [LDL] and Very Low-Density Lipoprotein [VLDL] was determined in 95 HIV positive subjects which include 48 patients who were on HAART- group 1 and 47 not on HAART- group 2; and compared to 30 HIV negative controls – group 3. Results: The level of TSH and fT3 was significantly (p < 0.05) higher in group 1 participants than in group 2 and the group 3 participants. The level of T4 was significantly higher in group 2 than in group 1 and group 3 participants. The level of T3 was significantly lower in Control participants in comparison to both HAART and non-HAART participants. The prevalence of fT4 dysfunction across the groups was significantly different from each other. The total mean of Cholesterol (163.5 ± 22.7), Triglyceride (163.5 ± 22.7), and Very Low-Density Lipoprotein (14.2 ± 2.4) of the HIV-positive participants were significantly (p < 0.05) lower than that of the HIV negative participants.Conclusion: The results obtained from this study indicate that serum levels of thyroid hormones may be used as baseline periodic markers during antiretroviral therapy and many people living with HIV may benefit from supplementation if appropriate.

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."