More Information
Submitted: January 22, 2022 | Approved: March 05, 2022 | Published: March 07, 2022
How to cite this article: ARSLAN K, TÖREL ERGÜR A, YİNANÇ MA. Overlap of two unusual condition in childhood: hibernoma and central diabetes insipidus. Ann Clin Endocrinol Metabol. 2022; 6: 001-003.
DOI: 10.29328/journal.acem.1001023
Copyright License: © 2022 ARSLAN K, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Overlap of two unusual condition in childhood: hibernoma and central diabetes insipidus
Kübra ARSLAN1* , Ayça TÖREL ERGÜR2 and Mehmet Ali YİNANÇ3
, Ayça TÖREL ERGÜR2 and Mehmet Ali YİNANÇ3
1Department of Pediatrics, Faculty of Medicine, Ufuk University, Turkey
2Department of Pediatric Endocrinology, Faculty of Medicine, Ufuk University, Turkey
3Department of Radiology, Faculty of Medicine, Ufuk University, Turkey
*Address for Correspondence: Dr. Kübra ARSLAN, Department of Pediatrics, Faculty of Medicine, Mevlana Boulevard No: 86-88, Dr. Rıdvan Ege Hospital, A Block, 3rd Floor, Pediatrics Service, Cankaya, Ankara, Ufuk University, Turkey, Email: [email protected]
Central Diabetes Insipidus (CDI) results from the inability to secrete ADH secreted by the neurohypophysis system to control water-electrolyte metabolism. In the etiology of CDI in childhood, many congenital and acquired central nervous system (CNS) tumors (germinoma, pinealoma, craniopharyngioma, optic glioma, acute myeloid leukemia), infiltrative diseases (Langerhans cell histiocytosis, sarcoidosis), infections (meningitis, tuberculosis, encephalitis), autoimmune events, head trauma, idiopathic) can be responsible [1]. Hibernomas, which are very rare in childhood, may also rarely involve the central nervous system.
Hibernoma is a benign tumor originating from brown adipose tissue. Brown adipose tissue is a fetal tissue for provides thermoregulation in newborns. Although it is found in a proportionally large amount in the neonatal period, it gradually decreases towards the adult period [2]. Brown adipose tissue is highly metabolically active, and it has been emphasized that it may contribute to the energy balance of the organism [3].
Like original tissue, the tumor is also metabolically very active [4]. It is mainly seen in the third decade of age and it is rarely seen in childhood [5,6]. Hibernomas are most common in the thigh, trunk, interscapular area, upper extremity, head, and neck [7]; however, there are case reports in the literature indicating that there may be many different locations in the body and that they may present with different clinical findings [5,8].
In this article, a case of CDI, which is thought to be due to an intracranial hibernoma, which is very rare in etiology, is presented and the approach and follow-up are discussed.
The twenty-month-old girl presented with complaints of excessive thirst and water intake and frequent urination for three months. There were no features other than head trauma two times in her history. Her general condition was good, anthropometric evaluation and physical examination were normal and her somatic development was appropriate for her age (Table 1). While there were no pathological findings in the biochemical parameters in the follow-up period, the urine output of the case was polyuric (11.68 ml/kg/h). The urine density was 1004 g/ml. The calculated polyuria limit was 900 cc/24 hours for her, but the 24 hour urine volume was 2900 cc, and the ratio of urine osmolarity to serum osmolarity (U/S osmolarity) was 0.27.
| Table 1: Anthropometric examination of the case. | |
| Age | 20 months |
| Puberty | P1 |
| Weight (kg) | 10.34 (25-50th percentile) |
| Height (cm) | 86.5 (75-80th percentile) |
| BMI | 13.77 (59th percentile) |
| Bone Age | Appropriate for age |
A water restriction test was applied to the patient to rule out psychogenic polydipsia. As a result of the test that was completed without any problems, it was observed that the urine density and ratio of U/S osmolarity of the patient did not increase (Table 2). The patient was diagnosed with diabetes insipidus (DI) when the serum antidiuretic hormone ADH level measured after the water restriction test was measured as 0.5 pmol/L. Desmopressin was given to the patient to determine whether the patient’s DI was central or nephrogenic. The patient, whose urine osmolarity increased more than 50% after desmopressin, was diagnosed as “Central Diabetes Insipidus”.
| Table 2: Biochemical and hormonal features. | |
| Case | |
| Complain | Excessive thirst and water intake and frequent urination |
| Urine density (g/ml) | 1004 |
| Poliyuria limit (cc/day) | 900 |
| Urinating (cc/day) | 2900 |
| Serum osmolarity (mosm/L) | 275 |
| Urine osmolarity (mosm/L) | 75 |
| Uosm/Sosm | 0.27 |
| Serum ADH (end of water restriction test) | < 0.5 |
| Uosm/Sosm (end of Desmopressin test - 2nd hour) | 0.95 |
| Increase of Uosm % (end of Desmopressin test) | > 50% |
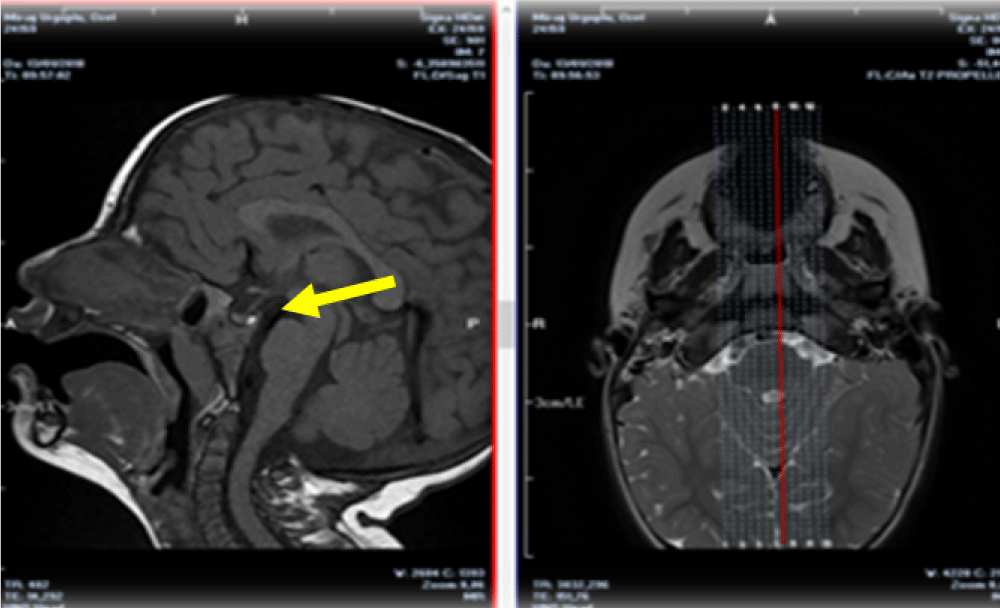
The blood biochemistry values of the patient were normal in etiological investigations. In pituitary MRI, there is a semisolid structure with protein and lipid content behind the neurohypophysis. This mass was approximately 2.5 mm x 2 mm in size which suggests that this formation led to a narrowing of the neurohypophysis volume. This appearance was found to match the characteristic MR appearance of hibernoma [8], and the lesion was evaluated in favor of choristoma-hibernoma (Figure 1).
Figure 1: The appearance of the lesion in MRI image.
Desmopressin treatment was initiated and the patient was followed up in terms of clinical and imaging.
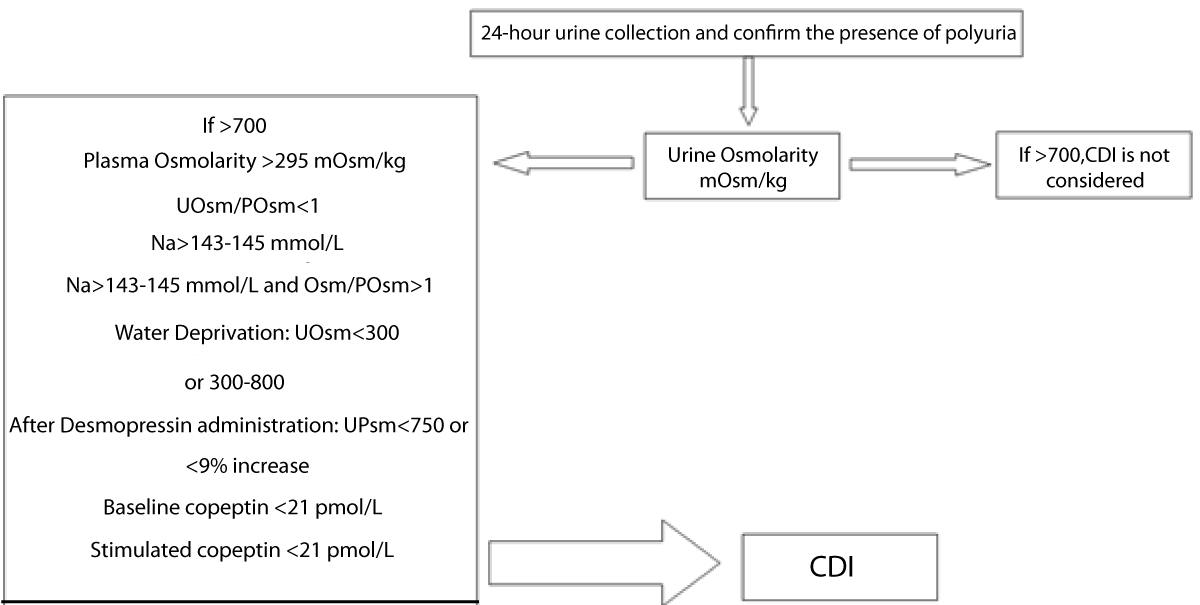
Central Diabetes Insipidus (CDI) is a very rare clinical condition with an average incidence of 3-4/100,000 in the general population. The prevalence of familial and congenital forms may change in childhood [10,11]. The pathogenesis of CDI is the destruction anyways neurons originating from the supraoptic and paraventricular nuclei in the hypothalamus. Different pediatric series were investigated. Eventually, the etiopathogenesis of CDI and the most common causes in the etiology are idiopathic causes, brain tumors, and brain malformations [1]. The physical examination can give an idea about the cause of the disease. Although the main symptoms are polyuria and polydipsia, different symptoms such as dehydration, growth-developmental delay, nocturia, constipation, aggression, and sleep disorders can be seen depending on the severity of the symptoms [12]. Our case had polyuria and polydipsia but no other clinical symptoms (dehydration, constipation, etc.) have been observed yet. Because her fluid intake was sufficient and she was diagnosed early. After polyuria was detected in our patient, tests were requested to make a differential diagnosis with the algorithm shown in Table 3 [12], and the patient was diagnosed with CDI.
Table 3: Algorithm for polyuria and polydipsia. Table prepared by Patti, et al. [1].
The first imaging method recommended after clinical diagnosis for etiology is magnetic resonance imaging (MRI) [12]. Pituitary MRI examination in our patient presented important findings in terms of CDI etiology. As described in the case report, a characteristic mass was detected in our case, which was thought to be compressing the neurohypophysis. The gold standard method for the diagnosis of hibernoma is pathological examination. However, its classic appearance in imaging may aid diagnosis and contribute to the regulation of treatment management. It gives an appearance between subcutaneous adipose tissue and muscle signal intensity in the T1 sequence and gives appearance with subcutaneous adipose tissue signal intensity in the T2 sequence in MRI [9,13,14].
It is very interesting that a 20-month-old baby has complaints of drinking too much water and frequent urination and being diagnosed with CDI with these complaints. In addition, even if the diagnosis of hibernoma is not confirmed pathologically in our case, the possible etiological factor detected in the etiology was hibernoma, which made our case even more interesting as it is the first in the literature. At this stage, considering the age of the patient, the size, and localization of the mass, the pathological examination was postponed to be performed in case of clinical findings that would require mass excision, in line with the ethical rule of “primum non nocere”. The patient improved with treatment and no enlargement of the mass was detected.
In the presence of suspicious lesions, total excision provides a cure for hibernoma and eliminates pressure effects [5]. The lesion detected in our case was in a difficult-to-reach area and its size was very small. There was no increase in size during follow-up and no additional symptoms were observed clinically and CDI that developed with the effect of compression responded to medical treatment. For this reason, the excision and pathological evaluation of the lesion, which has the appearance of a hibernoma, was postponed to later times.
Up to now, approximately 100 cases have been reported in the literature and 10% are located in the head and neck region [8,9]. However, the hibernoma of our case was in a very unusual place.
In addition, in cases with CDI, the bright spot normally seen in posterior pituitary MRI is expected to disappear [3,15]. An important detail in the evaluation of our case is that although CDI developed, the bright spot was seen on pituitary MRI. Although studies have reported that bright spots can be seen in early childhood in CDI [15], this finding in the posterior pituitary is a very important marker for CDI [16]. We want to emphasize again that clinically and laboratory correlation is very important for correct diagnosis. We also think that the follow-up of this patient in terms of mass size is a necessity because it may have cautionary value in terms of other hormone defects that can develop.
- Di Lorgi N, Napoli F, Allegri AEM, Olivieri I, Bertelli E, et al. Diabetes Insipidus – diagnosis and management. Horm Res Paediatr. 2012; 77: 69–84. PubMed: https://pubmed.ncbi.nlm.nih.gov/22433947/
- Mermer M, Acar Tek N. Adipose tissue and its effects on energy metabolism. Süleyman Demirel University J Health Sci. 2017; 40-46.
- Van Marken Lichtenbelt WD, Vanhommerig JM, Smulders NM, Drossaerts JMAFL, Kemerink GJ, et al. Cold-activated Brown adipose tissue in healty men. N Engl J Med. 2009; 360: 1500-1508. PubMed: https://pubmed.ncbi.nlm.nih.gov/19357405/
- Trujillo O, Cui IH, Malone M, Suurna M. An unusual presentation of a rare benign tumor in head and neck: a review of hibernomas. Laryngoscope. 2015; 125: 1656-1659. PubMed: https://pubmed.ncbi.nlm.nih.gov/25583551/
- Guidry CA, McGahren ED, Rodgers BM, Kane BJ. Pediatric cervicomediastinal hibernoma: A case report. J Ped Surg.2013; 48: 258-261. PubMed: https://pubmed.ncbi.nlm.nih.gov/23331827/
- Evers LH, Gebhard M, Lange T, Siemers F, Mailänder P. Hibernoma – Case Report and Literature Review. Am J Dermatopathol. 2009; 31: 685-686. PubMed: https://pubmed.ncbi.nlm.nih.gov/19668076/
- Honoki K, Morita K, Kasai T, Fujii H, Kido A, et al. Hibernoma of the axillary region: a rare benign adipocytic tumor. Rare Tumors. 2010; 2: 20-21. PubMed: https://pubmed.ncbi.nlm.nih.gov/21139952/
- Ahmed SA, Schuller I. Pediatric Hibernoma: A Case Report. J Pediatr Hematol Oncol. 2008; 30: 900-901.
- DeRosa DC, Lim RB, Lin-Hurtubise K, Johnson EA. Symptomatic hibernoma: a rare soft tissue tumor. Hawaii J Med Public Health. 2012; 71: 342-345. PubMed: https://pubmed.ncbi.nlm.nih.gov/23251871/
- Fujiwara TM, Bichet DG. Molecular biology of hereditary diabetes insipidus. J Am Soc Nephrol. 2005; 16: 2836–2846. PubMed: https://pubmed.ncbi.nlm.nih.gov/16093448/
- Patti G, Ibba A, Morana G, Napoli F, Fava D, et al. Central diabetes insipidus in children: Diagnosis and management. Best Pract Res Clin Endocrinol Metab. 2020; 34: 101440. PubMed: https://pubmed.ncbi.nlm.nih.gov/32646670/
- Rigoli L, Aloi C, Salina A, Di Bella C, Salzano G, et al. Wolfram syndrome 1 in the Italian population: genotype–phenotype correlations. Pediatr Res. 2020; 87: 456-462. PubMed: https://pubmed.ncbi.nlm.nih.gov/31266054/
- Little BP, Fintelmann FJ, Mino-Kenudson M, Lanuti M, Shepard JO, et al. Intrathoracic Hibernoma. A case with multimodality imaging correlation. J Thorac Imaging. 2011; 26: W20-22. PubMed: https://pubmed.ncbi.nlm.nih.gov/20871421/
- Mugel T, Ghoussain MA, Guinet C. MR and CT Findings in a case of hibernoma of the thigh extending into the pelvis. Eur Radiol. 1998; 8: 476-478.
- Ghirardello S, Garre ML, Rossi A, Maghnie M. The diagnosis of children with central diabetes insipidus. J Pediatr Endocrinol Metab. 2007; 20: 359–375. PubMed: https://pubmed.ncbi.nlm.nih.gov/17451074/
- Ghirardello S, Malattia C, Scagnelli P, Maghnie M. Current perspective on the pathogenesis of central diabetes insipidus. J Pediatr Endocrinol Metab. 2005; 8: 631-645. PubMed: https://pubmed.ncbi.nlm.nih.gov/16128239/