Table of Contents
Parathyroid Functions in Thalassemia Major Patients
Published on: 29th August, 2017
OCLC Number/Unique Identifier: 7317596427
Background: Hypoparathyroidism is well known to occur in thalassemia major patients, but it is thought to be uncommon and its incidence is considered to be decreasing with improvements in chelation therapy. The objective of this study was to assess the prevalence of parathyroid dysfunction in the first decade of life of the patients with thalassemia major.
Patients and Methods: Ninety children with beta-thalassemia major (55 males and 35 females) with a mean age of 7.17±3.78 years (1-13 years) and age and sex matched control group of 60 healthy children (36 males and 24 females) with a mean age 6.98±3.66 years (1-13) years. Serum parathyroid hormone (PTH), serum total Calcium (Ca), serum phosphorus (P), serum alkaline phosphatase (ALP), serum 25-hydroxyvitamin D (25-OHD) and serum ferritin levels were measured.
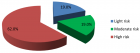
Result: PTH levels were higher than normal range in 23 (25.6%) patients with a mean value of 75.2±31.3 µg/mL compared to those having normal range level (35.3±15.2 µg/mL). Ca levels were found low in 11 patients (12.2%), and P levels were found high in 2 (2.22%) and low in 4 (4.44%) patients while high ALP levels were found in 6 (6.67%) patients. 25-OHD levels were low in all patients with a mean value of 24.95±5.82.
Conclusion: Reports in the literature indicate that parathyroid dysfunction due to iron overload generally occurs in 2nd or 3rd decade of patients with thalassemia major. However, our study shows that PTH due to iron overload may develop in a significant number of thalassemia major patients, therefore, all thalassemics should be carefully watched for endocrine organ function such as hyperparathyroidism might occur even in the first decade of the patients with thalassemia major.
Effect on Vitamin D status of Breastfeeding Infants after Vitamin D3 Supplementation during Breastfeeding Lactation: A double-blind randomized controlled trial
Published on: 4th August, 2017
OCLC Number/Unique Identifier: 7317627573
Background: Vitamin D deficiency in pregnancy increases several risks of breastfed mothers. To prevent these adverse events, vitamin D supplementation during pregnancy and lactation is recommended, but suggested dose ranges vary.
Objective: To determine whether vitamin D3 1,800 IU/d supplementation in lactating mothers improves the vitamin D status of their breastfed infants.
Materials and Methods: A randomized, placebo–controlled trial with Thai pregnant women was conducted. Lactating mothers (n=72) and their breastfed infants with insufficient maternal 25 hydroxyvitamin D (25(OH)D) levels in the third trimester were randomly assigned to two groups, one of which received 1,800 IU/d vitamin D supplementation and the other a placebo. Maternal serum 25(OH)D during lactation, cord blood, and 6-week breastfed infant serum were measured using LC-MS/MS.
Results: Mean maternal age (±SD) was 27±5 years, and pre-gestational BMI was 22.29±5 kg/m2. Maternal serum 25(OH)D at baseline was 22.29±7.15 nmol/L. At 6 weeks, both maternal 25(OH)D and infant 25 (OH)D levels had increased significantly in the vitamin D supplement group of mothers and infants (68.30±15.40, 40.40±12.56 nmol/L) compared to those in placebo groups (55.15±13.57, 24.28±17.20 nmol/L) (p <0.001, p<0.001). The changes in infant 25(OH)D levels increased substantially in the vitamin D supplement group but decreased in placebo(17.49±16.27 ng/ml compared to -1.34±19.23 nmol/L in the placebo group, p<0.001). The change of maternal 25(OH)D were positively correlation to the change of 25(OH)D level in breastmilk mothers and infants by r=0.697, p<0.001 and r=0.379, p=0.003 respectively.
Conclusions: Vitamin D3 supplementation to breastfed mother during lactation can increase serum 25(OH)D level in Thai breastfed mother and infants. Further work is needed to determine the optimum duration of vitamin D supplementation to normalized breastfed infants with 25(OH)D level >75 nmol/L.
Recurrent Cardiac Events Driven by Prothrombotic Burden in a Patient Undergoing Lipoprotein Apheresis for High Lp(a) Levels
Published on: 15th March, 2017
OCLC Number/Unique Identifier: 7317653746
Introduction: Lipoprotein (a) [Lp(a)] is a marker for cardiovascular disease, involved in pathogenesis and progression of atherosclerosis. In selected high-risk patients, lipoprotein-apheresis could optimize secondary prevention and improve prognosis.
Aim: We presented the case of a 49-year-old man with high lipoprotein (a) levels and recurrent cardiac adverse events, despite maximal pharmacological therapy.
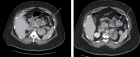
Case report: Four years before the admission at our Centre, he presented an anterior STEMI, treated with angioplasty and implantation of a drug eluting stent on left anterior descending artery, at the age of 47 years, in September 2012; one month later, the patients presented a new episode of angina, and exams showed a critical stenosis in the right coronary artery, treated by angioplasty and implantation of drug eluting stent. Because of high Lp(a) plasma levels, patient was subsequently on regularly 7-10 day lipoprotein apheresis.
Results and discussion: A thrombophilic screening was performed, showing the simultaneous presence of heterozygous V Leiden mutation and prothrombin G20210A mutation. He referred to our Centre in order to optimize therapy; we performed an endothelial function assessment showing a severe dysfunctional pattern.
Because of these findings, we prescribed dual antiplatelet therapy, and we added omega-3 fatty acids and association with nicotinic acid/laropiprant. According with current guidelines, considering the high risk of bleeding, we preferred not to administer anticoagulant therapy. At 6-month and 1-year follow up the patient continued lipoprotein apheresis and was asymptomatic for other cardiovascular events.
Conclusions: The assessment for the eventual presence of thrombophilia might become a useful tool in clinical practice for high-risk selected patients.

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."