More Information
Submitted: July 15, 2024 | Approved: July 30, 2024 | Published: July 31, 2024
How to cite this article: Popescu C, Șerbănescu MS, Calin G, Trăistaru MR. Physical Performance in the Overweight/Obesity Children Evaluation and Rehabilitation. Ann Clin Endocrinol Metabol. 2024; 8(1): 004-012. Available from:
https://dx.doi.org/10.29328/journal.acem.1001030
DOI: 10.29328/journal.acem.1001030
Copyright License: © 2024 Popescu C, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Child; Obesity; Physical performance; Rehabilitation
Physical Performance in the Overweight/Obesity Children Evaluation and Rehabilitation
Cristina Popescu1, Mircea-Sebastian Șerbănescu2, Gigi Calin3* and Magdalena Rodica Trăistaru4
1PhD Student, University of Medicine and Pharmacy in Craiova, Romania
2Department of Medical Informatics and Biostatistics, University of Medicine and Pharmacy in Craiova, Romania
3Pediatrics Department, University of Medicine and Pharmacy of Craiova, Craiova, Romania
4Department of Physical Medicine and Rehabilitation, Faculty of Nursing, University of Medicine and Pharmacy in Craiova, Romania
*Address for Correspondence: Gigi Calin, Lecturer, MD, PhD, Pediatrics Department, University of Medicine and Pharmacy of Craiova, 2 Petru Rareş Street, 200349 Craiova, Romania, Email: [email protected]
Introduction: Childhood obesity is one of the current themes of medical research, being considered not so much a multidimensional condition but primarily a real problem of worldwide interest.
The aim of our randomized study was to evaluate and compare the effects of physical exercise associated with an educational program on clinical-functional status in overweight and obese children.
Material and method: Participants were children hospitalized, through the emergency service, in the Pediatric Department, Craiova Municipal Clinical Hospital, between June and November 2023. 93 overweight and obese children, aged between 2 and 16 years, were evaluated (clinical, paraclinical and functional) by a multidisciplinary team and randomized into the control group (group C – 63 children) and the study group (group S – 30 children). After the resolution of the acute digestive or respiratory disease, the children in group S underwent a program to restore their functional status, based on educational measures (following the 5-2-1-0 rule) and physical exercises, for 12 weeks. Anthropometric data were measured (height, weight, body mass index); physical performance wasevaluated by gait analysis (we used the BTS G – WALK / BTS G – SENSOR 2 system, BTS Bioengineering Corp, Italy) with the determination of four parameters – the Timed Up-and-Go (TUG) test, the symmetry index, the walking test six minutes (6 MWT) and walking cadence or average cadence (steps/min) in both groups of children.
The results were obtained by analyzing the differences in values obtained in the two moments T1 (initial) and T2 (after three months). The proportion of girls and boys was approximately equal within obesity class in each study group. Although we did not obtain statistically significant differences between the monitored parameters, between the two groups, for the two evaluation moments, the children in Group S had a clearly favorable evolution for physical performance parameters, whose average value was improved in T2. Anthropometric data did not change.
Conclusion: The present study confirms the effectiveness of the multimodal (educational-kinetic) program for the physical performance of overweight/obese children. The sustained running of the program at home, with the involvement of the family and the school environment, is essential for the well-being of these children, with a favorable impact on the quality of life later.
Obesity is a complex multifactorial condition with numerous possible biological, behavioral and environmental determinants [1]. Many children are now growing up in an obese environment that promotes energy imbalance through the commercialization, availability and availability of energy-dense foods, along with decreased physical activity and increased sedentary screen-based activities [2].
Childhood overweight and obesity result from an accumulation of excess body fat and can increase the risk of health consequences both in the short term, but especially in the long term. In just 6 years, in 2030, it is estimated that almost 30% of all children will be overweight and obese [3]. The increase was higher until 2000 (as in adults), followed by a plateau, mostly in developed countries.
Since there are questions whether the standards of the World Health Organization (WHO) are useful for the population of children in Romania, synthetic growth references were developed in 2016 [4]. The authors used data from six studies with anthropometric information obtained between 1999 and 2016. If this synthetic reference is compared with the WHO and CDC (Centers for Disease Control and Prevention) references, there are statistically significant differences. Romanian children are taller than the WHO and CDC references and may have a BMI (Body Mass Index) higher than the WHO and IOTF (International Obesity Task Force) references [4]. There were some limitations to this reference, one being that it was created mainly from studies of urban children [4].
The fundamental principles of weight management in children and adolescents are the same as in adults (ie, reduced energy intake and increased energy expenditure), with the main goal being weight loss or slowing weight gain. Intervention approaches vary and depend on the child’s age and degree of overweight, among other considerations. Family-based interventions combining diet, physical activity and behavioral components have been shown to be effective and are considered current best practice in the treatment of childhood obesity in children under 12 years of age [5].
Regarding physical activity, there are numerous studies evaluating the association between physical activity and overweight and obesity in children and adolescents [6].
These studies found a positive correlation between reduced physical activity (exercise - walking, swimming, running, jogging and outdoor sports - volleyball, football, cricket, badminton and table tennis) and overweight and obesity. In these studies, time children’s activity times were generally shorter than 30 minutes per day and less than 2 hours per week [7].
Taking into account the importance of a kinetic program adapted to the child patient with overweight / obesity, we followed its effects, associated with educational measures, for physical performance and the development of a walking scheme as normal as possible. The child requires the adoption of a walking scheme as correct as possible, for a further harmonious development of posture and body alignment.
For a reporting of the results of our study to the literature data, the educational measures explained and recommended were those included in the 5-2-1-0 rule (5 or more vegetables and fruits, sitting in front of the TV/computer for less than 2 hours, physical activity for at least 1 hour per day and zero sugary drinks) seems to be the easiest recommendation [8].
Ethics approval
Before being included in the study, the details of the present research were explained to the child patients and their parents. Parents or guardians gave written informed consent.
The protocol was carried out in accordance with the Declaration of Helsinki and good clinical practice and was approved by the independent local ethics committee (opinion no. 38/01.03.2022).
Study design
Our prospective randomized study was conducted in the Departments of Pediatrics and Physical Medicine and Recovery, Filantropia Hospital, Craiova between June 2023 and November 2023.
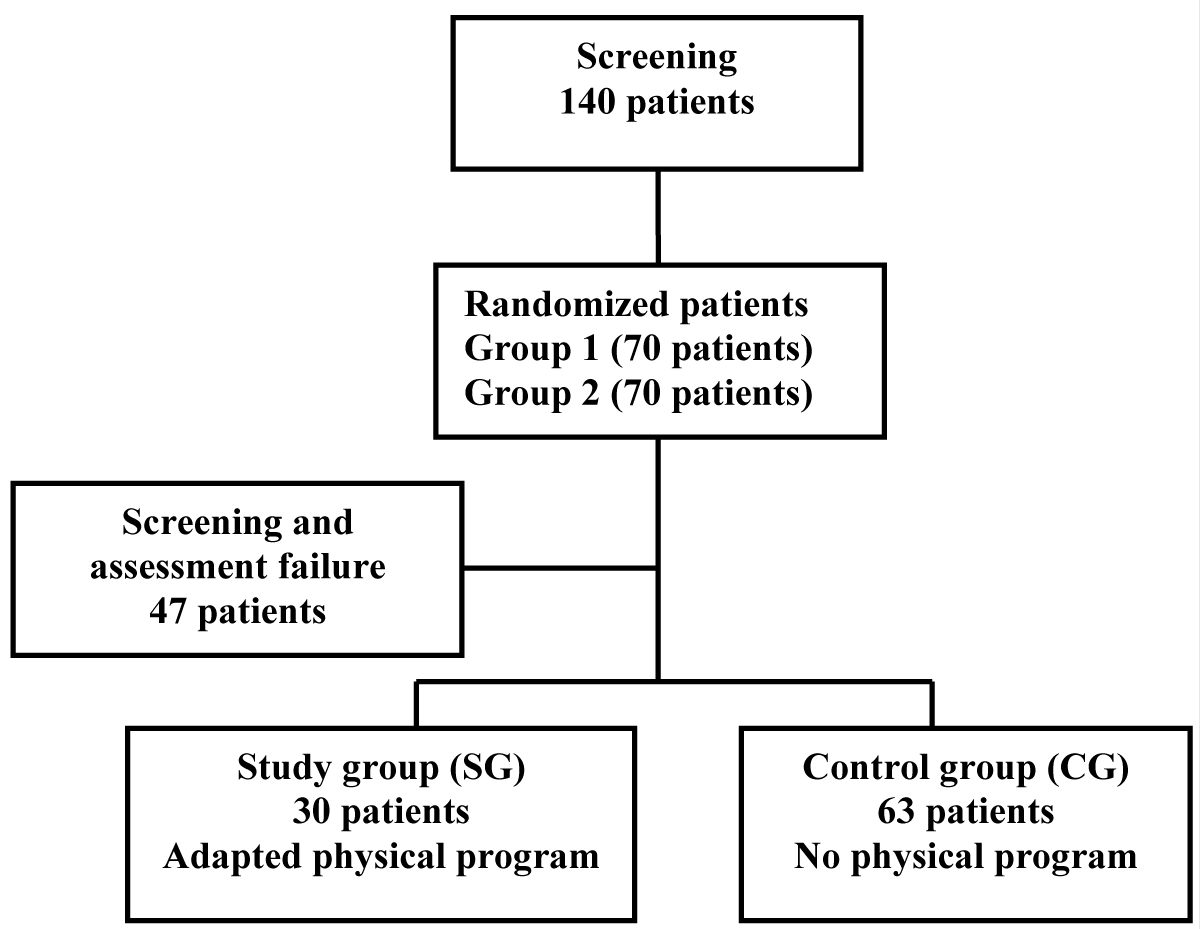
From 140 overweight and obese children, aged between 2 and 16 years, selected from admissions in the Pediatric Clinic, evaluated (clinically, paraclinically and functionally) by a multidisciplinary team, 93 were randomized to the control group (group C – 63 children) and the study group (group S – 30 children). The criterion for randomization was expressed willingness to participate in the kinetic program. After the resolution of the acute digestive or respiratory condition, the children in group S underwent a program to restore their functional status, based on educational measures (following the 5-2-1-0 rule) and physical exercises adapted to the age group and the patient’s compliance, while for 6 weeks. Those in the control group continued their daily activities similar to before hospitalization, but they were instructed to follow the 5-2-1-0 rule (Figure 1).
Figure 1: Diagram of our study.
The inclusion criteria in the study were:
- Above normal value of the Body Mass Index (BMI)
- The absence of another condition (cardiac, respiratory, digestive, hematological, renal, neurological with an impact on the ability to exercise)
- The expressed consent of the child and in writing of the parent/guardian
The evaluation of the children was done initially (T1) at the beginning of the study and after 3 months (T2). The following parameters were taken into account - anthropometric data and physical performance tests. I note that the full clinical and paraclinical (laboratory – screening tests) evaluation of each child preceded the targeted evaluation for the study.
Anthropometric data measured were height, weight, BMI = weight (kg)/height² (m) being calculated.
Body weight (kg) was measured using an electronic scale with a scale of 0 to 150 kg and an accuracy of 100 g. Standing height was measured using a portable stadiometer with an accuracy of 0.1 mm. During the measurement, the children were barefoot and with the least amount of clothing possible (only a light shirt and shorts).
All anthropometric variables were assessed twice by a single rater.
Physical performance testswere evaluated by gait analysis using a BTS G–WALK / BTS G – SENSOR 2 wireless system (BTS Bioengineering Corp., Italy), consisting of an inertial sensor composed of a triaxial accelerometer, a magnetic sensor and a triaxial gyroscope worn by the patient allows a functional gait analysis. We considered four clinical gait parameters: the Timed Up-and-Go (TUG) test, symmetry index, six-minute walking distance (6 MWD), and average cadence (steps/min).
Each child was explained the correct way to perform each physical performance assessment test and was familiarized with the equipment used. Standardized verbal encouragement was provided throughout the test to encourage peak performance.
The Timed Up-and-Go (TUG) test: The child sitting on a chair, gets up from the chair, walks at a safe and comfortable pace 3 meters (distance marked with a line), crosses the line, turns and returns to the chair, without assistance in walking. The time spent performing this task was recorded. We found the TUG to provide accurate information for gait stability, balance transitions from sitting to standing, and changes in gait.
Symmetry Index (SI): This index represents the subject’s ability to accelerate the center of mass in a similar manner during the right and left step cycle. The closer the index gets to 100, the more symmetry there is during the path. In general, non-pathological subjects show an index greater than 90. The symmetry index reflects the patient’s ability to have an identical pattern of acceleration and deceleration of the center of mass, regardless of the side of the gait cycle.
The six-minute walking test (6 MWT) was performed indoors [9] along a corridor (20 m long) that was marked every 2 m with a brightly colored tape. The starting and ending points of the walking route were marked by 2 cones, at the starting point and the ending point. Each child was tested individually and asked to walk the longest possible distance in 6 minutes (6 MWD). Only standardized expressions were used for encouragement (“keep going” and “going well”) and the announcement of time remaining. The six- minute test is simple, easy to apply, cheap and extremely effective in assessing the effort capacity.
Walking cadence represents the number of steps taken per minute by both legs (steps/minute). At a certain number of steps, a faster cadence and a shorter step length lead to the distribution of forces on all the joints of the lower limbs, with the achievement of a painless biomechanical balance, especially in conditions of excess weight.
Kinetic program (of adapted physical training) (Table 1): It consisted of physical activity for 60 minutes three times a week for 12 weeks, concurrent with the regular physical education hours that each child had provided in the appropriate schooling form.
| Table 1: The kinetic program indicated to the children in the study group. | ||
| Kinetic objective | Description | |
| 5 minutes warm-up - free walking, with balance of the upper limbs | ||
| Flexibility exercises | Waltz steps or other agreed dance | Daily, 10 minutes |
| Gymnastic exercises / jumping rope, rolling | Daily, 10 minutes, 5 sets of 2 minutes. | |
| Aerobic exercises (restoring / maintaining the ability to exercise, beneficial impact on the bone structure) |
Child-friendly sport (basketball, volleyball, tennis, swimming, running) |
60 min / session 3 sessions / week |
| House cleaning Bike ride ! for non-sports people |
60 min / activity 3 sessions / week |
|
| Walking coordination exercises | Walking in tandem Biofeedback in the mirror Walking the pet |
Daily, 10 - 15 minutes |
| 5 minute cool-down – easy running, stretching of the muscle groups of the lower limb | ||
| We did not indicate strength exercises, the children's age was under 16 years. Strength exercises are recommended in adolescents, after 16 years [11] |
||
It was held both indoors and outdoors depending on weather conditions. The program was adapted to each child in SG. Physical activity intensity was estimated by the physical therapist based on the children’s active behavior and was determined using the "Physical Activity Compendium” developed by Ainsworth, et al. [10].
Precautions have been taken to ensure the safety of children.
To ensure comparability between the different programs, the baseline exercise period followed a consistent principle of intensity control, whereby every 10 minutes of sports activities included at least 5 minutes of moderate to high intensity physical activity and 2 minutes of vigorous physical activity. The interventions were designed as games to increase children’s interest, the main differences being in the content of the basic exercises.
Statistical analysis
All quantitative data were summarized as mean and Standard Deviation (SD). We tested normality with the Kolmogorov-Smirnov test (p > 0.05 for all tests), and homogeneity of variances was assessed with Levene’s test.
Two-way repeated measures ANOVA was used to examine main effects and interactions for time (pre-test vs. post-test) and group (study lot vs. control lot) on selected outcomes. Following ANOVA, systematic post hoc paired-samples t-tests were performed to assess within-group changes over time for each measured variable.
We used a nonparametric paired samples t-test to assess differences before and after the training period for gait parameters.
Biserial rank correlation was used to estimate effect size, while a parametric paired sample Student’s t-test was used to assess the difference between gait parameter values before and after the training period, and Cohen’s d to assess effect size.
All significance was set at a p value of less than 0.05.
In Table 2 we have included the biographical and anthropometric data of the studied children.
| Table 2: Patient demographics. | |||||||
| Parameters demographer | Study lot (SG = 30 patients) | Control group (CG = 63 patients) | |||||
| Min | Max | Average (DS) | Min | Max | Average (DS) | ||
| BMI (Kg/m2) | 25.23 | 35.41 | 30.39 | 25 | 38.4 | 29.14 | |
| Age (years) | 5 | 16 | 9.83 | 2.7 | 16 | 7.93 | |
| Preschool (under 7 years old) = 23.33(%) Little schoolboy (7–10 years old) = 26.66(%) High school student (10–16 years old) = 50(%) |
Preschool (under 7 years old) = 44.44(%) Little schoolboy (7–10 years old) = 25.39(%) High school student (10–16 years old) = 30.15(%) |
||||||
| Gender | Girls | 39(65%) | 75(75%) | ||||
| Boys | 21(35%) | 25(25%) | |||||
| Own place | Urban | 31(51.67%) | 53(53%) | ||||
| Rural | 29(48.33%) | 47(47%) | |||||
The average age of both groups is close (9.83 years for SG, 7.93 years for CG), difference of only 1.39 years between the average values. This difference probably explains the higher compliance for physical activity in SG patients. The patients fall into the age groups of 5 years - 16 years, in both groups, without significant differences, p < 0.01481.
The urban/rural numerical ratio was 17/13 (1.30) for SG, respectively 30/33 (0.90) for CG without significant differences.
In SG (study group) there are 16 girls, representing 53.33% of children and 14 boys representing 46.66%, and the ratio of girls/boys is relatively equal, the difference is 2 children for girls. In CG (control group) there are 27 girls (42.85) and 36 boys (57.14), the girls/boys ratio is favorable to boys, the difference being 9 children.
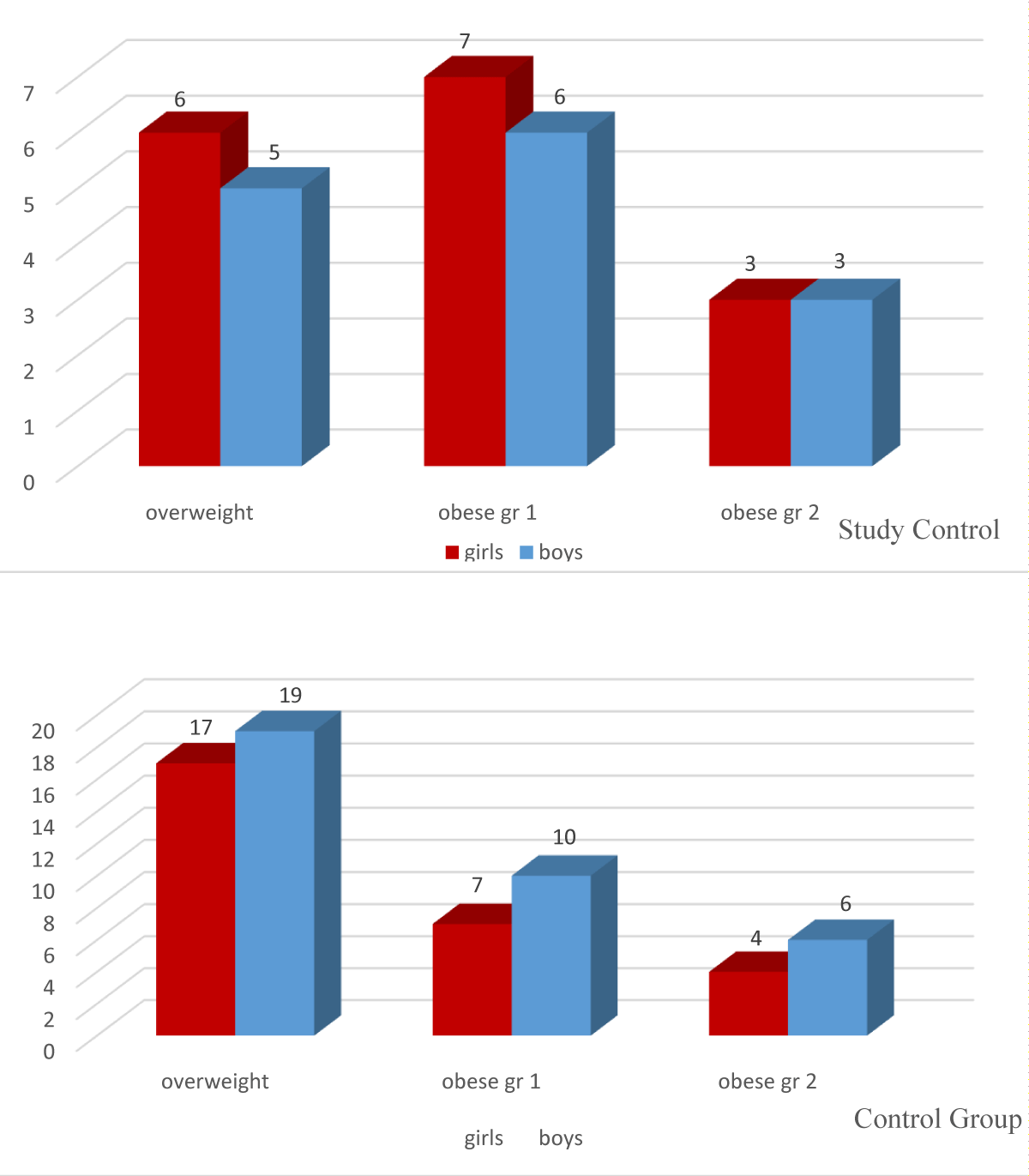
According to BMI, the children were divided into obesity classes:
- Overweight (6 girls and 5 boys), obese grade 1 (7 girls and 6 boys), obese grade 2 (3 girls and 3 boys), for SG;
- Overweight (17 girls and 19 boys), obese grade 1 (7 girls and 10 boys) and obese grade 2 (4 girls and 6 boys), for CG.
It is observed that the proportion of girls and boys is approximately equal (difference of 2 children) within the obesity class in each study group, the difference being more in girls in CG and less in SG (Figure 2).
Figure 2: Classification of children by obesity and gender groups.
Analyzing the BMI according to the environment of origin and gender, we found that there were no statistically significant differences, which means that there is no influence of the area of residence on the condition studied.
This is also observed within the schooling groups (Table 3).
| Table 3: BMI values according to demographic data. | |||||||
| Study group BMI = 30.39 | Control group BMI = 29.14 | ||||||
| Boys | Girls | Boys | Girls | ||||
| 30.30 | 30.50 | 29.01 | 29.25 | ||||
| Urban | Rural | Urban | Rural | ||||
| 30.01 | 30.89 | 29.65 | 28.69 | ||||
| pre-school | Small school children | High school students | pre-school | Small school children | High school students | ||
| 32.32 | 28.29 | 31.94 | 28.43 | 29.62 | 29.11 | ||
Physical performance tests
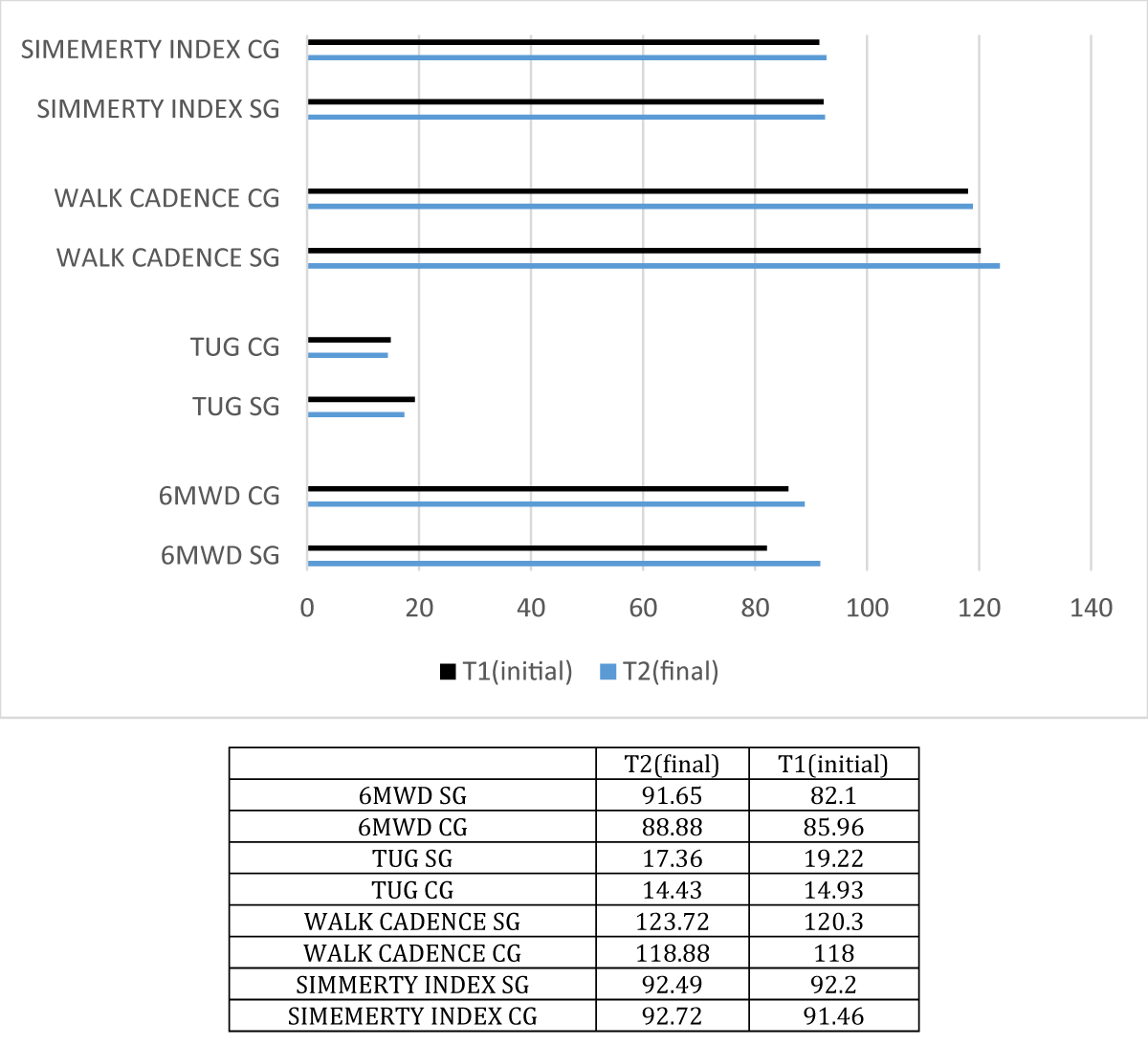
Comparing the initial values with the final ones, for each batch, we obtained the following results:
- The 6MWD: for SG the mean was 82.098 meters, initial and 91.69 meters final and p < 0.002397, which shows a statistically significant difference, and for CG, the values were insignificant, the mean was 85.96 meters initially and 86.13 meters final, p < 0.954061;
- TUG: the mean values in T2 were improved compared to T1, for the two groups, without a significant difference between the values (p = 0.285906, for SG and p = 0.70061, for CG);
- Walking cadence: mean values in T2 were improved compared to T1, for children from SG; in CG, the value was relatively similar in T2, even lower, without a significant difference between the values (p = 0. 133671, for SG and p = 0. 747056, for CG);
- Symmetry index: improved for both groups, more importantly for SG, but there was no statistically significant difference (t-test, p > 0.05) for both groups.
Analyzing the differences between the values obtained between the patients in the two lot groups, we noticed that, at the time of T1, there was no statistically significant difference between the studied parameters. Finally, there were significant differences for two parameters – walking cadence and symmetry index (Table 4, Figure 3).
| Table 4: Physical performance parameters in both groups. | ||||
| Parameters / Physical performance | Mediate | Std. Dev. | p (t test) | |
| 6MWD1 | SG (30 children) | 82.10# | 10.64 | 0.17402 |
| CG (63 children) | 85.96 | 16.23 | ||
| 6MWD2 | SG (30 children) | 91.65# | 19.40 | 0.19755 |
| CG (63 children) | 88.77 | 18.30 | ||
| TUG1 | SG (30 children) | 19.22 | 18.83 | 0.0555914 |
| CG (63 children) | 14.93 | 2.63 | ||
| TUG2 | SG (30 children) | 17.36 | 18.64 | 0.39840 |
| CG (63 children) | 14.43 | 2.60 | ||
| WALK1 CADENCE | SG (30 children) | 120.30 | 12.74 | 0.12290 |
| CG (63 children) | 118 | 12.60 | ||
| WALK2 CADENCE | SG (30 children) | 123.72 | 13.28 | 0.02858 |
| CG (63 children) | 118.88 | 12.84 | ||
| SYMMETRY INDEX 1 | SG (30 children) | 92.20 | 3.90 | 0.44608 |
| CG (63 children) | 92.20 | 5.03 | ||
| SYMMETRY INDEX 2 | SG (30 children) | 92.78 | 3.69 | 0.04963 |
| CG (63 children) | 91.47 | 4.49 | ||
| # p (t-test) = 0.002397, CG = Control Group, SG = Study Group, 6MWD = The 6 Minute Test , TUG = The Timed Up-and-Go Test | ||||
Figure 3: Value of walking parametersfor the two groups at T1 and T2.
Analyzing physical performance according to gender, we found that there were no statistically significant differences between girls and boys, but the values in T2 were improved compared to T1. Positive differences were observed in both girls and boys who performed extracurricular physical activity, compared to girls and boys who performed compulsory school physical activity. There is no influence of the area of residence on the state of physical performance neither for girls nor for boys in the two groups (Table 5).
| Table 5: Physical performance according to gender and area of residence. | ||||||||||
| Study Group | Control Group | |||||||||
| Girls | Boys | Urban | Rural | Total | Girls | Boys | Urban | Rural | Total | |
| 6MWD1 | 78.54 | 84.76 | 84.25 | 80.15 | 82.10 | 83.94 | 88.29 | 85.26 | 86.88 | 85.97 |
| 6MWD2 | 87.31 | 94.91 | 94.13 | 89.40 | 91.65 | 87.14 | 84.99 | 87.99 | 83.71 | 86.14 |
| TUG1 | 15.49 | 14.51 | 22.48 | 14.97 | 19.23 | 16.03 | 22.88 | 14.43 | 15.39 | 14.93 |
| TUG2 | 14.90 | 14.08 | 19.96 | 13.96 | 17.36 | 12.83 | 22.54 | 13.89 | 14.93 | 14.43 |
| WALK CADENCE 1 | 123.71 | 117.75 | 121.75 | 118.99 | 120.30 | 108.19 | 119.57 | 119.00 | 106.31 | 113.50 |
| WALK CADENCE 2 | 127.24 | 121.09 | 125.30 | 122.29 | 123.72 | 103.31 | 120.61 | 114.68 | 107.08 | 111.38 |
| SYMMETRY INDEX 1 | 90.12 | 92.48 | 90.58 | 92.28 | 91.47 | 93.91 | 90.24 | 92.10 | 92.33 | 92.20 |
| SYMMETRY INDEX 2 | 91.77 | 93.71 | 92.06 | 93.62 | 92.88 | 78.09 | 90.86 | 87.39 | 79.68 | 84.05 |
The group of high school students, following the application of the kinetic program, had positive results superior to the other age groups in all walking parameters, especially in the 6-minute test (6MWD in T2 was 102.28, compared to T1 - 90.67). The age group with a weaker but positive evolution was that of young schoolchildren, for all walking parameters (Table 6).
| Table 6: Physical performances for the age groups of the two groups. | ||||||||
| Study Group | Control Group | |||||||
| pre-school | Small school children | High school students | Total | pre-school | Small school children | High school students | Total | |
| 6MWD1 | 76.83 | 80.28 | 90.67 | 82.10 | 88.33 | 79.27 | 91.68 | 85.97 |
| 6MWD2 | 84.38 | 89.51 | 102.88 | 91.65 | 92.00 | 75.85 | 94.44 | 86.14 |
| TUG1 | 17.09 | 14.17 | 13.90 | 19.23 | 16.33 | 16.69 | 22.21 | 14.93 |
| TUG2 | 16.54 | 13.65 | 13.48 | 17.36 | 12.88 | 14.37 | 21.10 | 14.43 |
| WALK1 CADENCE | 133.22 | 119.56 | 107.85 | 120.30 | 129.67 | 117.92 | 105.93 | 113.50 |
| WALK2 CADENCE | 137.00 | 122.91 | 111.00 | 123.72 | 131.33 | 111.92 | 106.61 | 111.38 |
| SYMMETRY INDEX 1 | 85.77 | 93.51 | 94.15 | 91.47 | 87.67 | 92.34 | 93.04 | 92.20 |
| SYMMETRY INDEX 2 | 87.56 | 94.93 | 95.12 | 92.88 | 89.33 | 86.01 | 81.10 | 84.05 |
Also established the correlations of physical performances with age and BMI, at the time of T2, in order to orient ourselves on the effect of the applied kinetic program. The results obtained were:
- There is a reasonable correlation between the 6MWD parameter and children's age for both SG (r = 0.414) and CG (r = 0.498). For BMI there is a weak correlation for both groups (r = 0.379 for SG and r = 0.169 for CG).
- There is no correlation between the TUG parameter and the age of the children in the two groups, the correlation coefficient (r) being 0, and for BMI there is a weak correlation, r having values between 0.2 - 0.4;
- For both groups there is a weak negative association between the WALK CADENCE parameter and age (r = - 0.780 for SG, r = - 0.760 for CG). BMI has a weak correlation for SG (r = 0.373) and a very weak correlation for CG (r = 0.019);
- SYMMETRY INDEX has a weak negative correlation with both groups in terms of BMI (r = -0.117 for SG and r = - 0.139 for CG), age having a weak negative correlation for SG (r = -0.010) and reasonable for CG (0.501).
These correlations justify the complexity of conditioning the physical performance parameters, age and BMI not being the only variables with influence on their values.
The pilot study carried out on overweight / obese children for the analysis and monitoring of physical performance after the application of a kinetic program confirmed the essential role of physical activity for the state of health and the development of a scheme of walking as normal as possible in this category of child patients.
Associated with the kinetic program, we recommended compliance with the 5-2-1-0 rule, which we consider essential in the child’s metabolism and homeostasis [8].
Childhood obesity comes from poor nutrition education, especially by parents. Diet that has a high content of salt, sugar and fat, in combination with reduced physical activity is the main cause of obesity in children. And for these reasons, the treatment of childhood obesity is considerably difficult. Children’s poor motivation and parents’ inability to give them time have been reported as the most important factors causing low effectiveness of treatment in children and adolescents [8].
It is well documented that frequent physical activity has a positive impact on the development of motor coordination and general physical health in children [12].Exercise is a crucial non-pharmacological intervention to alleviate the problems of overweight and obesity and associated comorbidities starting in childhood. Thus, physical exercise intervention can be considered a safe and economical choice for improving physical condition and executive functions or physical skills in children [13].
A 2020 study to improve the physical condition of preschoolers [14] investigated the impact of different exercises on physical fitness. Physical fitness was assessed using standardized tests (eg, long jump, 20-meter sprint, medicine ball throw). The structured multisport program fundamentally also involved fine motor skills and exercises based on ball games twice a week. As in our study, the control group was free from any scheduled exercise with the exception of the mandatory program in kindergartens, respectively school.However, exercise alone may not be enough to reduce weight [15].
The objective, instrumental evaluation with the BTS system of the most important physical performances in the overweight/obese child pre- and post-kinetic program, represents a pioneering activity. We did not find similar studies in the literature to refer to our results.
In recent years, there have been studies, using the same device (BTS G–WALK/BTS G – SENSOR 2 wireless system), for the assessment of the walking pattern of overweight/obese children, without reporting the variation of these parameters in relation to a kinetic program.
In 2019, the „fineness of walking” or „step-by-step symmetry” was assessed in overweight/obese children, aged between 7 and 14, by analyzing the Harmonic Ratio. Different walking parameters were analyzed, from the perspective of the acceleration movement of the trunk in the three planes of movement, the child being monitored using the BTS device [16].
The results of this study showed that the harmony ratio allows the objective characterization of walking symmetry, even when walking parameters do not show differences.
In 2023, the same gait harmony rate was assessed in obese and overweight children aged between 6 and 10 years, depending on walking speed, cadence, duration of double support and step length. The defining parameters of gait were relatively identical in overweight and obese children, but the harmony rate differed, similar to the previous study [17].
In our study, we used the symmetry index to assess the finesse when walking. I found that the value increased after the kinetic program, with the mention that all the children, regardless of the group, had values above 90.
We believe that the inclusion of gait control exercises in the kinetic program is particularly important for this category of children.
The benefit is supported by the statistically significant differences between the average cadence parameter and the symmetry index, for the two batches, at the final moment.
Although there is no difference for walking cadence between normal-weight and obese children, as stated in the literature [18], the kinetic program, the average value of this walking parameter.
The lack of correlations between walking parameters and the BMI value [19], as we obtained in the present study, is similar to the literature data, confirming the complexity of the biomechanics of walking in children, regardless of weight and BMI.
The other components of the program (play, gymnastics-type activities, aerobic training) were chosen according to the recommendations in the literature.
A recent study [20] showed that a noncompetitive play-based physical activity intervention induced significant improvements in muscle strength and motor skill, which included speed, agility, and movement coordination.
Several authors emphasize that cardiorespiratory fitness is one of the most important components of health-related fitness [21].
The inclusion of respiratory physiotherapy, an aspect we did not delve into in the present study, in the preventive and curative kinetic program for overweight/obese children aims to increase lung capacity, with better muscle oxygenation and preparation of the body for the next exercise [22].
Laframboise and deGraauw [23] reviewed published studies that analyzed the effectiveness of aerobic physical training in reducing body fat in schoolchildren and adolescents. Interventions lasting 8 months have been shown to produce more benefits than those lasting up to 8 weeks. The study carried out by us had a duration of 3 months.
The authors of another review, Atlantis, Barnes and Singh [24], demonstrated that aerobic exercises lasting 155 - 180 min/week are more effective in reducing fat than those lasting 120 - 150 min/week. From the point of view of the structure of the program, we followed the recommended sequence of exercises: exercises that promote self-confidence, with the perception of self-efficacy, exercises for the paravertebral and belt muscle groups, exercises for motor skills and the promotion of motor control. We did not include strength exercises because the age of the children studied (under 16 years) did not allow it [11].
Changes in the child’s body during growth affect motor power and performance, so it was necessary to plan the exercise according to the individual characteristics, age and gender of the child. Frequent short-term exercises are more fun and accessible forms of exercise (dance at home) for children and increase exercise adherence.
Adaptation of multimodal supervised strategies ensured attendance, active participation, and enjoyment, compensating for the lack of strict caloric restriction and low volume and frequency of exercise compared to exercise prescription guidelines for obesity,the feasibility and benefits of applying multimodal intervention, including multicomponent exercise and nutritional counseling supervised by exercise specialists in collaboration with pediatric gastroenterologists and trained nutritionists [25].
The benefits of multimodal strategies, involving nutritional interventions as well as exercise in obese children, have been reported in many reviews and meta-analyses [26].
Exercise plus diet is a good strategy, despite the fact that children need to be especially motivated to continue physical activity and do not like to follow strict rules about food and schedule.
Weight management strategies based on lifestyle changes and multimodal health educational interventions, reducing sedentary activities and promoting daily movement should be considered first-line therapy for childhood obesity, as other treatments such as very low-calorie diets, pharmacotherapy or bariatric surgery are not generally accepted as safe [27].
In the treatment of obese children, the multimodal dimension is also respected by the medical team that provides their assistance; the cooperation of paediatricians, psychiatrists (child-adolescent), rehabilitation, sports medicine, dietitians and physiotherapists will provide an increase in treatment compliance and positive results [28].
The 1:2 size of the two groups (SG:CG) justifies the child’s fear of running a physical activity program. Therefore, the child patient must be encouraged to actively participate in the therapy, to maintain the level of physical activity as constant as possible.
The kinetic program applied to a child, especially an overweight child, is successful if it is created, run and monitored by a team that communicates effectively. Throughout the course of the study, collegial relationships, confidentiality of research results, and professional secrecy were maintained.
Study limitations
We did not track children’s unorganized activities and inactivity on a daily basis that could have influenced physical condition and skill development, as well as compliance with the recommended 5-2-1-0 rule.
The relatively small size of the lots should also be considered a limitation; randomized studies on extended groups are needed to determine the real effects of a kinetic program, associated with educational measures to restore and maintain physical performance in overweight/obese children.
The study included children from a single geographic location and socio-economic environment, which limits the generalization of the findings to other categories. However, the study included both male and female children and of different age groups.
1. Assessing and monitoring the child’s body mass index is an easy and objective way to quantify the multimodal management of childhood obesity.
2. The introduction of programs to promote physical activity for children and adolescents that also include coordination exercises, adapted to the age group, allows maintaining a balanced walking scheme and carrying out daily physical performance.
3. The treatment of childhood obesity is difficult, the easiest way being prevention. Following the 5-2-1-0 rule (5 or more vegetables and fruits, sitting in front of the TV/computer for less than 2 hours, physical activity for at least 1 hour a day and zero sugary drinks) seems to be the easiest recommendation.
- Kopelman P, Jebb SA, Butland B. Executive summary: Foresight 'Tackling Obesities: Future Choices' project. Obes Rev. 2007;8 Suppl 1:vi-ix. Available from: https://doi.org/10.1111/j.1467-789x.2007.00344.x
- Kremers SP, de Bruijn GJ, Visscher TL, van Mechelen W, de Vries NK, Brug J. Environmental influences on energy balance-related behaviors: a dual-process view. Int J Behav Nutr Phys Act. 2006;3:9. Available from: https://ijbnpa.biomedcentral.com/articles/10.1186/1479-5868-3-9
- Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804-814. Available from: https://doi.org/10.1016/s0140-6736(11)60813-1
- Pascanu I, Pop R, Barbu CG, Dumitrescu CP, Gherlan I, Marginean O, et al. Development of synthetic growth charts for Romanian population. Acta Endocrinol (Buchar). 2016;12(3):309-318. Available from: https://doi.org/10.4183/aeb.2016.309
- Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;(1). Available from: https://doi.org/10.1002/14651858.cd001872.pub2
- Bülbül S. Exercise in the treatment of childhood obesity. Turk Pediatri Ars. 2020;55(1):2-10. Available from: https://doi.org/10.14744%2FTurkPediatriArs.2019.60430
- Kotian MS, S GK, Kotian SS. Prevalence and determinants of overweight and obesity among adolescent school children of South Karnataka, India. Indian J Community Med. 2010;35(1):176-178. Available from: https://doi.org/10.4103%2F0970-0218.62587
- Amed S, Shea S, Pinkney S, Wharf Higgins J, Naylor PJ. Wayfinding the Live 5-2-1-0 Initiative—At the Intersection between Systems Thinking and Community-Based Childhood Obesity Prevention. Int J Environ Res Public Health. 2016;13(6):614. Available from: https://doi.org/10.3390%2Fijerph13060614
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111-117. Available from: https://doi.org/10.1164/ajrccm.166.1.at1102
- Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575-1581. Available from: https://doi.org/10.1249/mss.0b013e31821ece12
- Taşkın G, Şahin Özdemir FN. The importance of exercise on children. Gazi J Phys Educ Sport Sci. 2018;23:131-141. Available from: https://dergipark.org.tr/tr/pub/gbesbd/issue/36374/336399
- Bai Y, Chen S, Laurson KR, Kim Y, Saint-Maurice PF, Welk GJ. The associations of youth physical activity and screen time with fatness and fitness: The 2012 NHANES National Youth Fitness Survey. PLoS One. 2016;11(1). Available from: https://doi.org/10.1371/journal.pone.0148038
- Zhang M, Garnier H, Qian G, Li S. Effect of 11 weeks of physical exercise on physical fitness and executive functions in children. Children (Basel). 2023;10(3):485. Available from: https://doi.org/10.3390/children10030485
- Popović B, Cvetković M, Mačak D, Šćepanović T, Čokorilo N, Belić A, et al. Nine months of a structured multisport program improve physical fitness in preschool children: A quasi-experimental study. Int J Environ Res Public Health. 2020;17(14):4935. Available from: https://doi.org/10.3390/ijerph17144935
- Cox CE. Role of physical activity for weight loss and weight maintenance. Diabetes Spectr. 2017;30(3):157-160. Available from: https://doi.org/10.2337%2Fds17-0013
- Cimolin V, Cau N, Sartorio A, Capodaglio P, Galli M, Tringali G, et al. Symmetry of gait in underweight, normal and overweight children and adolescents. Sensors (Basel). 2019;19(9):2054. Available from: https://doi.org/10.3390%2Fs19092054
- Porta M, Cimmino D, Leban B, Arippa F, Casu G, Fastame MC, et al. Smoothness of gait in overweight (but not obese) children aged 6-10. Bioengineering (Basel). 2023;10(3):286. Available from: https://doi.org/10.3390/bioengineering10030286
- Darwesh A, Hafez EA, Aboeleneen AM, El-Banna MF, El-Gendy SR. Three-dimensional gait analysis for spatiotemporal parameters in obese children. IOSR J Nurs Health Sci. 2018;7(3):11-16. Available from: http://dx.doi.org/10.9790/1959-0703081116
- Elazeem MRA, Eltohamy AM, Ali MS. Association between body mass index and spatial gait parameters in primary school children. Bull Fac Phys Ther. 2021;26:20. Available from: https://bfpt.springeropen.com/articles/10.1186/s43161-021-00037-9
- Martínez-Vizcaíno V, Pozuelo-Carrascosa DP, García-Prieto JC, Cavero-Redondo I, Solera-Martínez M, Garrido-Miguel M, et al. Effectiveness of a school-based physical activity intervention on adiposity, fitness and blood pressure: MOVI-KIDS study. Br J Sports Med. 2020;54(5):279-285. Available from: https://doi.org/10.1111/sms.14113
- Ruiz JR, Ortega FB, Gutierrez A, Meusel D, Sjöström M, Castillo MJ. Health-related fitness assessment in childhood and adolescence: a European approach based on the AVENA, EYHS and HELENA studies. J Public Health. 2006;14:269-277. Available from: http://dx.doi.org/10.1007/s10389-006-0059-z
- Ortega FB, Ruiz JR, Castillo MJ, Sjöström M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes (Lond). 2008;32(1):1-11. Available from: https://doi.org/10.1038/sj.ijo.0803774
- Laframboise MA, Degraauw C. The effects of aerobic physical activity on adiposity in school-aged children and youth: a systematic review of randomized controlled trials. J Can Chiropr Assoc. 2011;55(4):256-268. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3222701/
- Atlantis E, Barnes EH, Singh MA. Efficacy of exercise for treating overweight in children and adolescents: a systematic review. Int J Obes (Lond). 2006;30(7):1027-1040. Available from: https://doi.org/10.1038/sj.ijo.0803286
- Cordellat A, Padilla B, Grattarola P, García-Lucerga C, Crehuá-Gaudiza E, Núñez F, et al. Multicomponent exercise training combined with nutritional counselling improves physical function, biochemical and anthropometric profiles in obese children: a pilot study. Nutrients. 2020;12(9):2723. Available from: https://doi.org/10.3390%2Fnu12092723
- Kelley GA, Kelley KS, Pate RR. Exercise and adiposity in overweight and obese children and adolescents: a systematic review with network meta-analysis of randomised trials. BMJ Open. 2019;9(11). Available from: https://bmjopen.bmj.com/content/9/11/e031220
- Aikenhead A, Knai C, Lobstein T. Do surgical interventions to treat obesity in children and adolescents have long- versus short-term advantages and are they cost-effective? World Health Organization. Regional Office for Europe; 2012. Available from: https://iris.who.int/handle/10665/364519.
- August GP, Caprio S, Fennoy I, Freemark M, Kaufman FR, Lustig RH, et al, Endocrine Society. Prevention and treatment of pediatric obesity: an Endocrine Society clinical practice guideline based on expert opinion. J Clin Endocrinol Metab. 2008;93(12):4576-4599. Available from: https://doi.org/10.1210/jc.2007-2458